HELP US, HELP MOMS 💜 DONATE
What the Pump!?
Navigating breast pumping in early postpartum.
Lactation for Leaps & QueenCare
6/13/20244 min read
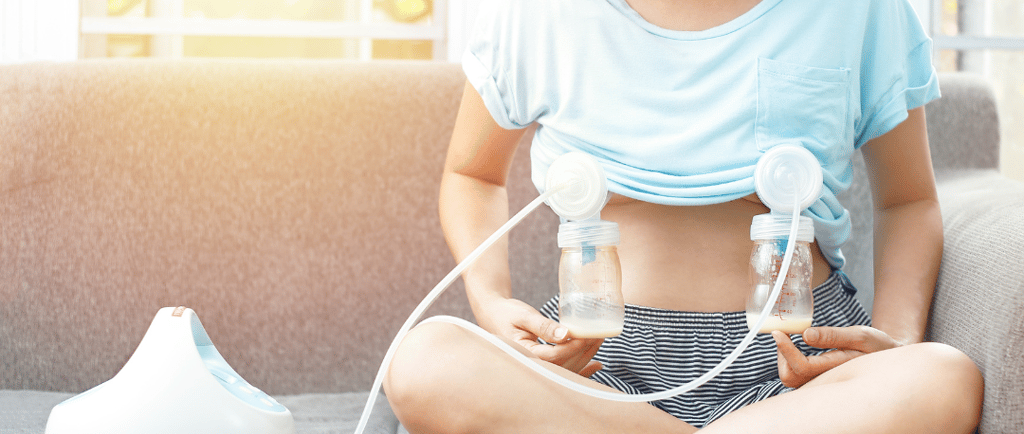
Breastfeeding is a learning curve on its own, and then we add pumping to the mix, and no wonder those early weeks of Motherhood can be overwhelming! We've teamed up with Lactation for Leaps to help navigate these challenges, and provide guidance on breastfeeding and how pumping fits into the real picture.
DO I NEED TO PUMP TO BREASTFEED SUCCESSFULLY?
NO! In fact, it takes about 6-8 weeks for the supply and demand relationship of breastfeeding to establish between mom and baby. It would be our best recommendation to hold off on pumping until after you and baby are comfortable with breastfeeding, and the supply/demand relationship has been well established.
WHAT ARE THE DOWNSIDES OF INTRODUCING PUMPING TOO EARLY?
The main risk with pumping during this stage is developing an oversupply. This is when your body produces far too much milk, causing most of the baby's feed to be what is known as foremilk, which is very high in lactose. This high lactose load is too much for the baby's immature GI system and causes an array of worrisome symptoms such as collicky behaviour, explosive green bowel movements, and excessive gas.
During the first 6-8 weeks of breastfeeding the breasts are very sensitive to both increasing and decreasing supply to meet the needs of your baby. Your body determines how much it needs to make based on how frequently and thoroughly the breasts are being drained, titrating the supply to adequately meet the supply and demand routine. The majority of mothers will make more than their baby requires in the first few weeks of lactation, making it important to allow your baby to guide the supply / demand relationship of milk supply, unless otherwise indicated by a healthcare provider.
WHAT IF I WANT TO CREATE A FREEZER STASH?
The fist 6-8 weeks should be focused on establishing a breastfeeding relationship that ensures good effective feeding at each feed and establishing milk supply, freezer stash comes later! However, our breasts naturally leak from both sides when feeding. You can collect this milk by placing a milk collector on the opposite breast during feedings. This is NOT the same as pumping, because it is not drawing the milk from the breast, just collecting the leakage that would be otherwise absorbed by your clothing or breast pad and wasted.if mothers want to collect letdown they should be catching without suctioning to the breast by tucking the device into the bottom of the bra to secure. *Haakaas and other systems that use suction are known to cause oversupply in mothers sensitive to oversupply as they still pull more than just the let down.
WHAT ABOUT PUMPING BEFORE BABY IS BORN?
You may have heard about moms that are pumping even BEFORE baby has arrived. Although this isn’t necessarily bad, remember that you are not yet producing milk before baby is born. What you will be pumping / collecting is colostrum, and although that stuff is LIQUID GOLD, by about day 3-4 your baby will be ready for breastmilk, and no longer feeding off of colostrum Most women’s milk comes in around day 3-4 postpartum
Collecting colostrum AFTER 38 weeks can be helpful to bring to the hospital after the baby is born to provide via spoon or syringe while the baby is learning to breastfeed as a "top up". Sometimes when baby and Mum are having a hard time getting onto breastfeeding, having the colostrum on hand can prevent early bottle feeding and formula. When used as a top up at the end of a feed it helps fill baby's belly up a bit more, which can give Mum a bit more rest between feeds.
SO, WHEN WOULD I NEED TO PUMP IN EARLY POSTPARTUM, AND HOW WOULD I KNOW?
- When baby is receiving a bottle rather than the breast for a feeding. If your baby is feeding 8-10 times a day, milk MUST be removed 8-10 times either by baby or pump if you are separated to protect the milk supply. This is true throughout your lactation journey.
- When baby is a "lazy feeder" or feeding ineffectively. Pumping the residual milk following the conclusion of a feed to ensure adequate drainage to protect your supply while you await lactation support to assist with increasing efficient feeding habits. Post-residual pumping will save your supply, but it is important that the baby is being encouraged to feed well to ensure adequate weight gain. When feeding is well established, post-residual pumping is no longer required and baby can adequately titrate the supply.
IF I WAITED UNTIL LATER, WHEN EXACTLY, AND HOW WOULD I INTRODUCE PUMPING?
When breastfeeding is well established after 6-8 weeks postpartum, starting a freezer stash of milk can safely begin. This can look like pumping directly after a feeding, which can be done up to every feed.
Up to 2 additional pumping sessions can be added each day, 1 hour after a feed. This allows time for your breasts to create milk while not "stealing" from the next feed.
Trying to keep your additional pumping sessions around the same time each day will help your body know and prepare to make more milk during that time of the day. It is important, even at this time, to monitor yourself and baby for symptoms of oversupply.
HOW DO I MAKE SURE I AM USING MY PUMP SAFELY?
1) Ensure proper flange size by measuring and following the sizing guide provided with your pump.
2) Use the lowest suction pressure needed to remove the milk. More suction DOES NOT mean more milk yield, it means increased chance of nipple trauma.
3) Only pump until the milk stops spraying and cap all pumping sessions at 10 minutes to prevent duct trauma.
4) Ensure soft pump parts are NEW if you have a used machine or are using a machine you used during a previous lactation period.
5) Ensure adequate cleaning of your pump parts based on manufacturer's recommendations.
6) Ensure safe milk storage.


